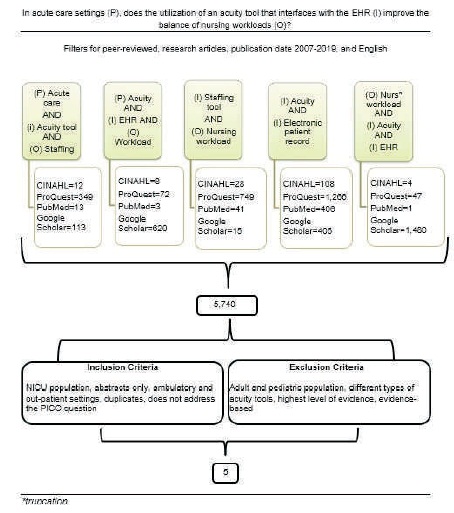
Figure 1. Search Flow Diagram
Matching nursing resources with patient needs and acuity while maintaining patient safety and quality of care has become increasingly difficult due to the increase in nursing shortage. Nurses have growing concerns about equity and satisfaction regarding patient assignments. The purpose of this project was to discover the effects of utilizing an acuity tool that interfaces with the Electronic Health Record (EHR) to accurately assess patient acuity and balance the nursepatient workload. A search plan was developed to identify keywords within several article databases. Existing literature identified evidence on how an electronic acuity-based staffing tool balances nurse-to-patient workload and allows for consistent, high-quality patient care while managing healthcare costs. An acuity measurement tool interfaced with the EHR can be an excellent resource for optimizing nurse staffing and workload. Electronically predicting a patient's acuity provides a powerful tool for healthcare managers to allocate resources. Such estimations and predictions on patient's acuity can be produced from vast amounts of electronic healthcare data, information technology, and computational intelligence techniques. Using tactical decision-making and resource allocation with different mathematical optimization models will support acuity predictions and help to balance nurse workloads.
Hospitals continue to face a shortage of nurses, which increases concerns of adverse effects on patient safety (American Association of Colleges of Nursing, 2017). Variations in the size and composition of nursing workloads influence patient safety and quality of care (Rosenberg, 2019). When staffing a nursing unit, assignments must take into consideration the acuity of patients. According to O'Keeffe (2016b), acuity-based staffing links to positive clinical and patient outcomes such as decreases in mortality and length of stay. Acuity-based tools use enhanced decision-making processes that maximize patient, nursing, and operational outcomes while improving patient and nurse satisfaction (O'Keeffe, 2016b). Patient acuity levels can be predicted based on health data interfaced with the EHR utilizing natural language processing along with a machine-learning algorithm, also known as an EHR acuity tool. Interfacing the electronic acuity tool allows a program that sits outside the EHR to communicate and interact with the EHR.
According to Jones, Whyley, Doyle, and Bevan (2018), there is evidence showing that lower nurse staffing levels and higher nurse workloads in acute care settings poorly affects patient outcomes with an increase in mortality, falls, infections, and hospital stays. Heavy nurse workloads are also associated with adverse effects on staff well-being. Nurses expect equitable patient assignments as each nurse shares the workload for all patients to receive safe and quality care. Acute care patients have more complex health issues and comorbidities than in previous decades. Nurses no longer focus on a list of tasks to be completed, instead; they focus on the patient and family as a complete unit (O'Keeffe, 2016a). Due to the increased complexity of patients' health, nurse workloads have increased; resulting in poor job satisfaction, decreased retention rates, poor patient outcomes, and inflated health care costs.
Accurate staffing also leads to a decrease in organizational costs of approximately $37,700 to $58,400 per nurse as well as an estimated $5.2 to $8.1 million annually on costs associated with marketing, hiring, and training (University of New Mexico, 2016). Technology has advanced the healthcare system to improve patient care and patient outcomes. Now is the time to use technology to advance towards equitable workload through the use of an acuity tool interfaced with the EHR. The purpose of this project was to discover the effects of utilizing an electronic acuity tool that interfaces with the EHR on accurate assessment of patient acuity to balance the nurse-patient workload. The PICO (Population (P), Intervention (I), Comparison (C), Outcome (O)) question driving this project was: In acute care settings (P), does the utilization of an acuity tool that interfaces with the EHR (I) improve the balance of nursing workloads (O)?
In order to evaluate the effects of utilizing an electronic acuity tool that interfaces with the EHR to balance nursepatient workload, a systematic review was performed to find relevant evidence (Figure 1). For the literature search, different library and internet databases were utilized to find appropriate evidence to answer the PICO question. The databases used were the Cumulative Index of Nursing & Allied Health (CINAHL), ProQuest, PubMed, and Google Scholar. The databases were searched simultaneously utilizing the same key search terms. Limiters were used to define the articles needed, including peer-reviewed, research articles, English, free full-text, and defined time frame from 2014-2019. Several different combinations of key search terms were utilized. Inclusion criteria in the search included adult and pediatric population, electronic and interfaced acuity tools with EHRs, paper acuity tools (for comparison), and a search for the highest level of evidence possible. The highest level of evidence is considered to be a systematic review followed by randomized controlled trials, controlled cohort studies, uncontrolled cohort studies, case studies, and descriptive studies followed lastly by expert opinions (Menlyk & Fineout- Overholt, 2015). Exclusion criteria included neonatal population, abstracts only, ambulatory and outpatient settings, and duplicate articles. Applying the inclusion and exclusion criteria narrowed the number of articles to a total of five that would help to address the need for an electronic acuity tool that interfaces with the EHR.
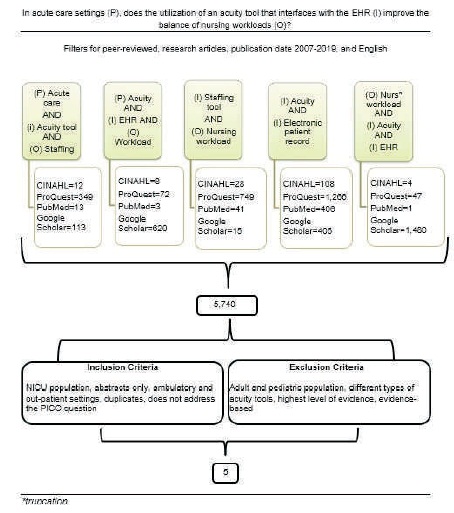
Figure 1. Search Flow Diagram
The resulting five articles were critically appraised by three or more authors who are clinical nurse experts. The authors examined the factors related to the utilization of an acuity tool interfaced with the EHR and the rigor of each study (Table 1).
To assign nursing staff for patient care, most organizations use volume-based and reimbursement-driven methods (Gelinas, 2016). Nursing workload is contingent on the work environment, acuity of patients, and nursing turnover rates. Patients have varying care needs and treatment plans resulting in different nurse-to-patient workloads. Paperbased and electronic acuity nursing workload tools that are not interfaced with the EHR have been used in different acute care settings (Giammona et al., 2016). These tools need to be completed by a nurse by hand, which can take time to complete. The articles showed how an electronic acuity-based staffing tool interfacing with the HER balances nurse-to-patient workload and allows for consistent, high-quality patient care while managing healthcare costs.
Giammona et al. (2016) developed and implemented a Nursing Care Score (NCS) system built into the Electronic Health Record (EHR) to evaluate if the NCS system would alleviate additional nursing tasks of documenting in a separate workload system. Results showed enhanced nursing satisfaction and fair distribution of nursing work tasks among staff. Equitable nursing workload distribution can lead to improving job satisfaction, retention, and a decrease in burnout among nursing staff (Giammona et al., 2016). The quality improvement initiative confirmed that using a nursing workload measurement tool built into the EHR did not increase nurse workload and improved distribution of nursing work tasks among staff.
Kontio et al. (2014) identified the need to use electronic medical records to determine patient acuity scores in order to help reduce health care costs, improve nursing workloads, health care budgets, and allocate resources more appropriately. This study showed that by using free text documentation and previously assigned acuity scores, it was possible to predict a patient's acuity score for the following day.
Larson et al. (2017) examined different nurse care procedures to develop and test a Nursing Intensity of Care Index (NICI) using available electronic data from the EHR. The project showed that the NICI tool was beneficial in measuring the nursing intensity or acuity of nursing needs, however, the tool was not interfaced with the EHR. The NICI scores were compared to clinical expert's manual assessments and were found to be similar to the NICI scores. The NICI tool aided in lowering nurse workloads and could be interfaced into the EHR. Using this information from the EHR develops evidenced-based information about real-time effectiveness of interventions. Further development of this tool may positively impact patient safety needs and infection prevention practices, as well as, have financial impacts for institutions.
Massarweh, Tidyman, and Luu (2017) implemented a Quality Improvement (QI) project that led to the design and development of an eAssignment sheet tool that interfaces with patient electronic information to assist nurse managers in equitable workload distribution. Successful testing of the eAssignment sheet supported the validity of the QI project, however, was not interfaced with the EHR. According to Massarweh, Tidyman and Luu (2017), data-enabled technology informs decision-making and moves the nursing profession towards proper electronic acuity-based nurse-to-patient staffing and away from opinion-based staffing processes.
Young, Lee, Sands, and McComb (2015) sought to determine which nursing activities and factors are influential in nursing staffing decision-making. The reviewed established 20 workload measurement tools and extracted 1,438 activities, after a second reviewer eliminated duplicate and redundant activities, the 1,438 activities were decreased to 502 nurse care activities. The 502 nurse care activities were incorporated into a comprehensive survey. Ninety percent of nurse managers completing the survey reported only using 21 nurse activities out of the 502 nurse activities. No individual measurement tool contained all 21 nurse activities, which may explain why there have been doubts about the reliability of current nurse workload measurement tools and why available tools may be underutilized. The study confirms that a standardized approach, such as a Nurse Workload Measurement tool, interfaced into the hospital information system, would optimize nurse staffing, therefore balancing nurse workload.
The research that has been completed inferred that using an electronic acuity tool that interfaces with the EHR can promote equitable workload distribution, predict nursing intensity and patient acuity, improve patient safety by decreasing sentinel events, manage healthcare costs, and improve nurse satisfaction (Giammona et al., 2016; Kontio et al., 2014; Larson et al., 2017; Massarweh et al., 2017; & Young et al., 2015).
Limitations were identified in the literature review. Due to the lack of research, information was limited related to an acuity tool that interfaces with the EHR focused on improving the balance of nursing workloads. One electronic acuity tool that can be utilized by different types of nursing units may pose challenges due to the various patient acuities. In addition, countries have different healthcare standards, therefore, acuity tools would vary and may not be applicable. The literature found was lower level research and quality improvement projects.
A recommendation for further research involves addressing several different geographical regions within the United States and distinct patient populations, such as cardiac, orthopedic, and neurologic (Young et al., 2015). Nurse leaders, nursing staff, patients, and their families, all gain to profit from an interfaced EHR acuity tool. Through cost reduction, staff retention, increased patient satisfaction scores, decreased adverse events, and increased reimbursement cost, organizations will see the benefits of an electronic acuity tool to balance nursepatient workloads. Once a comprehensive electronic acuity tool that interfaces with the EHR is developed, a study will need to be developed on a larger scale, comparing the effectiveness of the tool at a minimum of ten hospitals, urban and rural, to depict a more expansive picture on the efficacy of balancing nurse workloads. Utilizing an electronic acuity tool interfaced with the EHR can be costly due to the start-up costs, training staff, and the continued yearly costs for upkeep (Dyrda, 2016). Many of these costs may be alleviated with an increase in nurse satisfaction, which can decrease turnover rates and marketing costs
Nurses play a critical role in determining patient safety, quality of care, and patient outcomes. Education needs to be provided to current nursing staff on the acuity tool that is interfaced with the EHR. Nurses will need to understand the importance of real-time and accurate documentation to ensure balanced nurse workloads. Nursing administration is responsible for ensuring that nurses have an adequate work environment to provide quality care to patients and their families, this includes the development of the software needed to ensure appropriate resource planning and staffing for high acuity settings. Promoting the implementation of utilizing an electronic acuity tool interfaced with the EHR will impact organizational cost savings, improving patient and nurse satisfaction, and decreasing the overall turnover rate (Massarweh et al., 2017).
synthesis of the evidence shows that it is possible to predict a patient's acuity utilizing an electronic acuity tool interfaced with the EHR. However, additional research involving higher levels of evidence should be conducted. With the nursing shortage expected to continue and patients acuity rising, it is critical that patient health data within the EHR be utilized to predict staffing. Using specialized software interfaced with the EHR makes the process for acuity-based staffing faster and more accurate than paper staffing workload assignments and allows for tactical decision-making. The findings show that utilizing an electronic acuity tool interfaced with the EHR can accurately predict patient acuity and help to balance nurse workload. Technology can match the right nurse with the right patient at the right time.