Figure 1. Conceptual Frame Work based on Callista Roy's Adaptation Model (1984)
Lower respiratory tract infection is common among children. This will interrupt the children breathing pattern and cause breathing difficulty. This study was carried out to assess the effectiveness of Strelinikova breathing exercise on reduction of respiratory signs among preschooler with Lower respiratory tract infection. The study was based on Callista Roy's adaptation model of nursing theory. Quasi experimental pretest and posttest control group design has been adopted. The study was conducted in Agasthiya Muni Child Care Centre, Vellamadam. Purposive sampling technique was adopted. A sample of 30 was selected on the basis of inclusion criteria, from 15 experimental group, 15 control group preschooler with lower respiratory tract infection. The data collection tool included demographic variables and Modified severity of exacerbation grade scale and oxygen saturation. Strelinikova breathing exercise was demonstrated by investigator to the experimental group for 10 - 15 minutes. This was followed for five days and was given thrice a day. Posttest was conducted on 5th day in both experimental and control group. In part I in the experimental group the pretest mean respiratory sign score was 6.06 with SD 1.66 and in the control group, the mean score was 5.86 with SD 1.60. The mean difference was low and statistically not significant. That is both groups are equal in the pretest level of respiratory signs. In the experimental group, posttest means respiratory signs score was 3.66 with SD 0.72 and in the control group was 4.93 with SD 1.27. The mean difference was high and statistically significant. That is the Strelinikova breathing exercise was effective in part I respiratory signs. In part II in the experimental group, the pretest mean respiratory sign score was 2.60 with SD 0.51 and in the control group, the mean score was 2.46 with SD 0.52. The mean difference was low and statistically not significant. That is both groups are equal in the pretest level of respiratory signs. In the experimental group, posttest means respiratory signs score was 1.33 with SD 0.52 and in the control group was 1.83 with SD 0.45. The mean difference was high and statistically significant. That is the Strelinikova breathing exercise was effective in part II respiratory signs. The findings revealed that the administration of Strelinikova breathing exercise has a better effect in reducing lower respiratory tract infection.
Today's society is complex and ever changing. As children grow they must not only cope with current demands, but also prepare for many unexpected events they would face tomorrow. Changes brought by new techniques and technologies will continue to have an impact on society as a whole (WHO, 2011). Breathing is an uninterrupted bodily activity that controls the mental and emotional responses of the body. In today's fast paced life, where people hardly has time to relax, most of them suffer from anxiety, stress, depression, etc. Detailed studies of the past have shown that majority of individuals do not properly make use of the entire capacity of respiratory organs, i.e. while breathing one use only a small portion of their lungs, which leads to insufficient supply of oxygen to the lungs. This further gets stressed by their slothful and strained lifestyle, which leads to many complications like headaches, asthma, wheezing, chest pain, fatigue, etc. By implementing the breathing exercises, one can get rid of these complications and live a healthy lifestyle. The solution to this is to take out some spare time from ones’ busy daily routine to perform these deep breathing exercises. Healthy children brought up in healthy surroundings, not only are the source of joy to everyone, but will also be India's greatest resource of tomorrow. Children are in a dynamic process of growth and development, and are particularly vulnerable to acute and chronic effects of pollutants in their environment, which leads to diseases like Acute Respiratory Infections (ARI), diarrhea, etc. Among these infectious diseases, LRTI is one of the leading causes of mortality and morbidity in young children (Weigl et al., 2005). Lower Respiratory Tract Infections (LRI) inflict a high burden of disease in children worldwide. Longitudinal descriptive epidemiological data on different forms of LRI are urgently needed to differentiate this burden. Population was compared based on incidence rates between countries and recognize trends. From July 1996 to June 2000, many children were hospitalized with LRI, i.e., lar yngotracheao bronchitis, Wheezing Bronchitis, Bronchiolitis (WBB), bronchopneumonia, and pneumonia in the municipal area of Kiel Schleswig Holstein, Germany were analyzed by cross sectional studies. In the four year observational period, 1072 children aged 0 to 16 years (median 23 months) were hospitalized with LRI. 12% (median 28 months) with LTB (larynx, trachea, bronchus), 11% (median 17 months) with bronchitis, 28% (median 13 months) with WBB, 26% (median 26 months) with bronchopneumonia, and 22% (median 47 months) with pneumonia. The prevalence of chronic underlying conditions (20%) and low gestational age (13%) varied in different forms of LRI. The cumulative incidence rate of LRI rate increased steadily over 4 years (Edwin, 2009). A study in Trichy on “planned teaching programme on practice of ARI among mothers of under-five children”. The study was conducted with a sample of sixty mothers of children with ARI. The study found that there was gross inadequacy of knowledge regarding ARI among mothers and health education imparted to the mothers had an effect on their knowledge and attitude of practice regarding ARI. The findings of the result were as follows: in case of knowledge, the mean difference was 48.4 and paired 't' test was 38.32, for attitude of the mothers, the mean difference was 4.76 and paired 't' test was 11, and for knowledge on practice, mean difference was 4.83 and paired 't' test is 10.06 and the p value was found to be p<0.05. Hence the study concluded that the planned teaching programme was found to be effective in improving the knowledge, attitude, and knowledge on practice of mothers regarding acute respiratory infections. There was a gross inadequacy (100%) of knowledge regarding ARIs among mothers in both the groups. PTP was found to be effective in improving the knowledge, attitude and knowledge on practice of mothers regarding ARIs as shown by the posttest scores of experimental group. Considering the above review, the researcher felt the need to assess the level of knowledge on expected practices regarding home management of respiratory problems and enhance the knowledge with planned teaching programme. Study recommended that a study regarding prevention and risk factors of ARI should be done in the community and descriptive study can be done to assess the knowledge, attitude and knowledge of practices (Flower & Saewyc, 2005). A study was done on assessing the capability of school-age children with asthma to safely self-carry an inhaler in Golden Valley (Breathing exercise for Children with Asthma, 2016). It is a descriptive study. Asthma Assessment Interview (AAI) was used as a tool. A random sample of 34 students with asthma from a mid western school district were interviewed by the school nurse using the AAI, which assesses knowledge of asthma, symptoms, coping strategies, medication administration skills, triggers, and judgment about when to use an inhaler including the ability to tell time. Only 38% passed the AAI. No students ages 5 to 7 passed, fewer than 50% of students ages 8 to 10 passed, and half or more of students age 11 or older passed the AAI. Results suggest a school nurse should supervise elementary students when using an inhaler; most should not self-carry. The AAI can be a useful part of the school nurse's assessment (Jobsis, Schellekens, Kroesbergen, Hop, & De Jongste, 1999). A study to compare exhaled NO concentrations considered as the method of choice, with 2 sample methods that are easily performed by children 100 and 1 well controlled, stable allergic asthmatic children (median age 11.7 years) was performed. 29 children (29%) were not able to perform a constant flow exhalation of at least 3 s. NO concentrations (means plus or minus SEM) were 5.3+0.2 parts per billion (ppb) at the endexpiratory plateau, 5.2+0.3 ppb in balloons (intra class correlation co-efficient (ri) = 0.73) and 8.0+0.4 ppb during tidal breathing (p<0.001, ri =0.53 compared to plateau values). Mean values of NO during tidal breathing increased significantly with time. It was concluded that in asthmatic children, the end expirator y plateau concentration of NO during exhalation at 20% of the vital capacity per second is similar to values obtained if the balloon method (Larson, & Kim, 1984). A study at Cheltenham and the aim of this pilot study was to assess the effect of preoperative inspiratory muscle training on respiratory variables in patients aged between 6-18 years undergoing major abdominal surgery during the study. Pulmonary functions and Respiratory muscle strength by maximum inspiratory and expiratory mouth pressure were measured at least two weeks before surgery in 80 patients waiting for the major abdominal surgery. Patients were then allocated randomly to one of the four groups (Group A, control; Group B, deep breathing exercises; Group C, incentive spirometry; Group D, specific inspiratory muscle training). Patients in Groups B, C, and D were asked to train twice daily, each session lasting 15 min, for at least two weeks before surgery. Outcome measurements were made immediately pre-operatively and postoperatively. Finally, the study stated that pre-operative respiratory muscle strength and expiratory mouth pressure prevents lung complications during the postoperative period (Westerdahl, Lindmark, Eriksson, Hedenstierna, & Tenling 2005). A study to investigate the effects of deep-breathing exercises on pulmonary function, atelectasis, and arterial blood gas levels after surgery in Sweden was done. A prospective, randomized trial study with patients performing deep-breathing exercises (n = 48) was compared to a control group of (n = 42) who performed no breathing exercises postoperatively. The patients in the deep-breathing group were instructed to perform breathing exercises for the first 4 postoperative days hourly during daytime. The exercises consist of 30 slow, deep breaths performed with a positive expiratory pressure blowbottle device. Post-test by spirometric measurements, spiral CT arterial blood gas analysis, were performed on the fourth postoperative day. Control subjects compared to the patients in the deep-breathing group had a significantly smaller reduction in FEV1 (to 71 ± 11%, vs 65 ± 13% of the preoperative values; p = 0.01) and FVC (to 71 ± 12%, vs 64 ± 13% of the preoperative values; p = 0.01), and 72% of the patients experienced a subjective benefit from the exercises. Children those performing deep-breathing exercises after surgery had significantly smaller atelectatic th areas and better pulmonary function on the 4 postoperative day when compared to the control group performing no exercises (Ritz, Meurets, Wilhelm, & Roth, 2009). An experimental study to evaluate the effect of Buteyko breathing technique among twelve asthmatic children of age group 6-12 years was conducted in Southern Methodist University, USA. During the 4th -week training, patients in the treatment group (n=8) showed stable, increases in PCO2 and reductions in respiration rate. In control patients (N=4), symptoms and physiological parameters remained stable during the 4-week wait period. The study concluded that the Buteyko breathing technique was significantly improved in PCO2, respiration rate, and symptoms were gradual across the four weeks of training (Saini, Gaur, Saini, & Lal, 1992). A descriptive study was done to correlate acute respiratory tract infection ARI among under five in the selected area of the Udupi district. 110 mothers and their children above 1 year were selected for the study. A structured interview schedule was used for data collection. Majority of children that is 60.9% had ARI 4 to 6 times in the past three months. During one-month observation, maximum number of children, 48.6% had at least suffered from ARI once. Chi-square values computed between an occurrence of ARI and selected variables revealed a significant association between the occurrence of ARI and physical health of the infant and environment pollution. The study showed that the majority of children suffered 4 to 6 times with respiratory tract infection in three months of study period.
A Study to assess the effectiveness of Strelinikova breathing exercise on reduction of respiratory signs among preschooler with Lower respiratory tract infection in selected hospital at Kanyakumari District (Strelinikova breathing exercise, n.d).
H1: There will be a significant difference between mean pretest and posttest scores of Strelinikova breathing exercise in experimental group and control group.
H2: There will be a significant association between pretest level of respiratory signs with their selected demographic variables among experimental group and control group.
It refers to determining the extent to which the breathing exercise has brought significant difference in reducing the respiratory signs among preschooler.
It refers to 5 exercises, such as Palms, Shake of hands, Pump, Hug the shoulder, Head turns. Each exercises is done by maintaining proper position and then making short loud sniffs strongly. The exercise programme includes 5 exercises, done 3 times daily in the morning, afternoon, and evening for 5 consecutive days. Each exercise is done in first portion of 4 sniffs, then a short pause, it is continued till 16 sniffs. Each session includes 10-15 minutes.
It refers to the children of the age group 36 to 72 months with Lower respiratory tract infection.
Wheezing, breathlessness, rapid breathing, and cough are some prominent signs of Lower Respiratory Tract Infection (LRTI). And it is identified through respiratory rate, presence of wheezing, and usage of accessory muscle measured by severity and exacerbation grade scale and oxygen saturation.
It refers to preschooler with LRTI, bronchitis, bronchiolitis, asthma, pneumonia admitted in an inpatient department in Agasthiya Muni Child Care Centre, Vellamadam, TamilNadu, India.
4.5.1 Assumption
4.5.2 Limitation
The conceptual framework of the present study is adapted from the Callista Roy's adaptation model (1984) and is shown in Figure 1. Roy explained that adaptation occurs when people respond positively to environmental changes and it is the process and outcome of individuals and groups who use conscious awareness, self reflection, and choice to create human and environmental integration.
Research approach used to accomplish the objectives of this study was quantitative approach based on testing a theory composed of variables measured with numbers and analyzed using statistical techniques.
The research design selected for this study was quasi experimental with pretest and posttest control group design to measure the effectiveness of Strelinikova breathing exercises.
The study was conducted in Agasthiya Muni Child Care Centre, Vellamadam, which is nearly 20 km from Christian College of Nursing, Neyyoor.
The population of this study was preschooler with Lower Respiratory Tract Infection in Agasthiya Muni Child Care Centre, Vellamadam at Kanyakumari District.
In this study, the sample size consisted of 15 experimental and 15 control group (total 30 sample) with Lower Respiratory Tract Infection.
Preschooler with Lower Respiratory Tract Infection who satisfied the inclusion and exclusion criteria were selected using purposive sampling technique.
The sample was selected based on the following criteria;
The study included the samples with the following traits.
Preschooler who were
The study excluded the following characteristics.
Preschoolers who were
In this study, the dependent variable was Lower Respiratory Tract Infection among preschooler.
In this study, independent variable was Strelinikova breathing exercise.
The following instruments were prepared and used by the investigator for data collection.
The study had two parts of tool.
Part: I
Demographic and clinical variables such as Age (in months), Sex, Education, Parents education, Parents occupation, family monthly income, Chief complaints to respiratory signs, Duration of hospitalization, Area, Pet animals in house, Type of allergy.
Part: II (a)
Modified Severity and exacerbation grade scale to assess the respiratory signs (adapted from IAP Respiratory chapter, 2003). It includes respiratory rate, wheezing present, and accessory muscle usage.
Part: II (b)
Oxygen Saturation (Table 3).
In this study, the context of the instrument was validated by experts in the field of pediatrics. Tool validation was done with the experts; 2 pediatricians, 3 experts in the field of child health nursing (Tables 1 and 2).
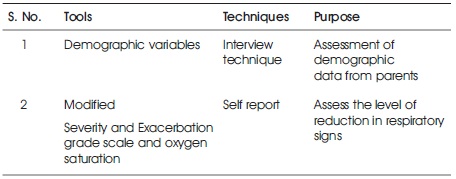
Table 1. Tools Validation
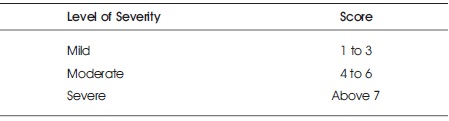
Table 2. Level of Severity and Score
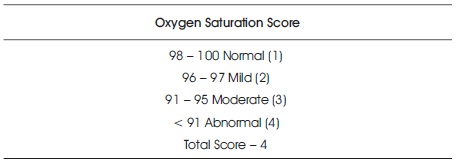
Table 3. Oxygen Saturation Score
In this study, reliability of the tool was obtained by interrater method.
In order to test the feasibility, relevance, and practicability of the study, the pilot study was conducted in Kanyakumari Medical Mission Hospital, among 3 sample subjects. After the approval from the concerned institution, oral consent was obtained from the subjects after explaining the purpose of the study. The level of reduction of respiratory signs was assessed before and after administering Strelinikova breathing exercise by using modified severity exacerbation scale and oxygen saturation. The result of pilot study revealed that the study was feasible.
The main study was conducted at Agasthiya Muni Child Care Centre, Vellamadam. Data collection was done for a period of 6 weeks. Before conducting the study, formal permission was obtained from Dr. Sudha Ponnu MBBS, MD (Pediatrician) at Agasthiyar Muni Child Care Centre, Vellamadam.
The data was collected in the following steps
After obtaining the required permission from the concerned authorities and informed consent from the parents, the investigator introduced herself, explained the purpose of the study, and collected the data pertaining the demographic variables. The study was conducted in the following phases.
Phase 1: The investigator assessed the respiratory parameters, which includes, respiration rate, breathe sounds, accessory muscles, and oxygen saturation by using pulse oximeter, stethoscope, and observation in both experimental and control group.
Phase 2: Strelinikova breathing exercise was demonstrated by investigator to the experimental group for 10 - 15 minutes. This was followed for five days and was given thrice a day. There was no intervention for the control group.
Phase 3: After the end of the intervention (5th day), posttest score of respiratory parameters was assessed by using pulse oximeter, observation, stethoscope in both experimental group and control group.
The data collected was analyzed by means of descriptive statistics and inferential statistics.
Permission was obtained from the institution and concerned authorities before data collection. An informed consent was obtained from mothers of preschooler children admitted with respiratory signs. Privacy and confidentiality was maintained.
The study was conducted after the approval from the dissertation committee of Christian College of Nursing, Neyyoor. Formal administrative permission was obtained from Dr. Sudha Ponnu, MBBS., MD (Pediatrician), Agasthiyar Muni Child Care Centre, Vellamadam. Oral consent was obtained from the subjects before starting the data collection. Assurance was given to the study subjects that anonymity of each individual would be maintained. This was done for assuring the normal and ethical as well as for the legal safety of the investigator.
Table 4 shows that there is no association between the pretest level of part-I respiratory signs among the preschooler with their selected demographic variables like sex, parents education, parents occupation, family monthly income, area of living, type of allergy except age, education, chief complaints to respiratory signs, duration of hospitalization, pet animals in house in the experimental group and control group. Table 5 shows that there is no association between the pretest level of part-II respiratory signs among the preschooler with their selected demographic variables like sex, parents education, parents occupation, family monthly income, area of living, type of allergy excepts age, education, chief complaints to respiratory signs, duration of hospitalization, pet animals in house in the experimental group and control group.
Table 4. Determine the Association between Pretest Part I Level of Severity of Respiratory Signs with Selected Demographic Variables in both Experimental and Control Group
Table 5. Determine the Association between Pretest Part II Level of Severity of Respiratory Signs with Selected Demographic Variables in both Experimental and Control Group
In group I, majority of the sample subjects 7 (46.67%) were in the age group of 61-72 months, 5 (33.33%) were in the age group of 49-60 months, and 3 (20.00%) were in the age group of 36-48 months.
In group II, majority of the sample subjects 6 (40.00%) were in the age group of 61-72 months, 5 (33.33%) were in the age group of 49-60 months, and 4 (26.67%) were in the age group of 36-48 months.
In group I, majority of the sample subjects 8 (53.33%) were female and 7 (46.6 7) were male.
In group II, majority of the sample subjects 8 (53.33%) were female and 7 (46.6 7) were male.
In group I, majority of the sample subjects 10 (66.67%) were 1 std, 5 (33.33%) were UKG.
In group II, majority of the sample subjects 9 (60.00%) were 1 std and 6 (40.00) were UKG.
In group I, majority of the sample subjects 8 (53.33%) were graduate and 7 (46.67%) were higher secondary.
In group II, majority of the sample subjects 8 (53.33%) were higher secondary and 7 (46.67%) were graduate.
In group I, majority of the sample subjects 7 (46.67%) were non-government, 5 (33.33%) were self-employee, and 3 (20.00%) were government.
In group II, majority of the sample subjects 8 (53.33%) were non-government, 4 (26.67%) were self-employee, and 3 (20.00%) were government. In group I, income of majority of the sample subjects, 7 (46.67%) were 10,001 - 15,000/-, 6 (40.00%) were 5000 - 10,000/-, 2 (13.33) were 15,001 - 20,000/-.
In group II, income of majority of the sample subjects 7 (46.67%) were 5000 - 10,000/-, 6 (40.00%) were 10,000 - 15,000/-, 2 (13.33) were 15,001 - 20,000/-.
In group I, majority of the sample subjects 5 (33.33%) were with cough and wheezing, complaints of wheezing with fever 4 (26.67), 4 (26.67%) were with breathing difficulty and wheezing, and 2 (13.33) were with cough with fever.
In group II, majority of the sample subjects 5 (33.33%) were with breathing difficulty and wheezing, 4 (26.67%) were wheezing with fever, 3 (20.00%) cough and wheezing, and 3 (20.00%) cough with fever.
In group I, majority of the sample subjects with duration of hospitalization 7 (46.67%) were 1-3 days, 7 (46.67%) were 4-5 days, 1 (6.66%) were above 5 days. In group II, majority of the sample subjects with duration of hospitalization 8 (53.33%) were 1-3 days, 7(46.67%) were 4-5 days.
In group I, majority of the sample subjects 8 (53.33%) were living in urban and 7 (46.67%) were living in rural area.
In group II, majority of the sample subjects 8 (53.33%) were living in rural and, 7 (46.67%) were living in urban area.
In group I, majority of the sample subjects 8 (53.33%) were pet animals in house and 7 (46.67%) were No pet animals in house.
In group II, majority of the sample subjects 8 (53.33%) were No pet animals in house and 7 (46.67%) were pet animals in house. In group I, majority of the sample subjects 6 (40.00%) were No allergy 4 (26.67%) were dust allergy, 4 (26.67%) were house mites allergy, and 1 (6.66%) food allergy.
To assess the pretest level of respiratory signs of preschooler with lower respiratory tract infection in both experimental and control group.
In the pretest majority of the sample subjects, 8 (53.33%) had moderate level of exacerbation grade 7 (46.67%) had severe level of exacerbation grade. No one had mild exacerbation grade in the experimental group.
In the pretest majority of the sample subjects, 8 (53.33%) had severe level of exacerbation grade, 7 (46.67%) had moderate level of exacerbation grade. No one had mild exacerbation grade in the control group.
In the pretest majority of the sample subjects, 8 (53.33%) had moderate level of oxygen saturation, 7 (46.67%) had mild level of oxygen saturation. No one had Normal and severe level of oxygen saturation in experimental group.
In the pretest, the majority 8 (53.33%) had mild level of O2 saturation, 7 (46.67%) had moderate level of O2 saturation. No one had Normal and severe level of O2 saturation in control.
To assess the posttest level of respiratory signs of preschooler with Lower Respiratory Tract Infection after giving Strelinikova breathing exercise in experimental group.
In the posttest, majority of the sample subjects, 8 (53.33%) had moderate level of exacerbation grade, 7 (46.67%) had mild level of exacerbation grade. No one had severe exacerbation grade in the experimental group.
In the posttest, majority of the sample subjects 10 (66.67%) had moderate level of exacerbation grade, 3 (20.00%) had severe level of exacerbation grade, and 2 (13.33%) had mild level of exacerbation grade in the control group.
In the posttest, the majority of the sample subject 8 (53.33) had mild level of oxygen saturation, 7 (46.67%) had normal oxygen saturation. No one had moderate and severe in oxygen saturation in experimental group.
In the posttest, the majority of the sample subject 11 (73.33%) had mild level of oxygen saturation, 4 (26.651%) had Normal level of oxygen saturation. No one had moderate and severe level of oxygen saturation.
To compare the pretest and posttest score on respiratory signs of preschooler children with lower respiratory tract infection in experimental group and control group.
The part-I pretest mean score of respiratory signs was 6.06 with SD 1.66 and in the posttest score was 3.66 with SD 0.72. The mean difference was high and statistically significant in the experimental group.
In the control group, the pretest mean score was 5.86 with SD 1.60 and in the post test score was 4.93 with SD 1.27. The mean difference was high and statistically significant. This is due to the normal treatment.
In Part -II, the pretest mean score of respiratory signs mean was 2.60 with SD 0.51 and in the post test SD mean score was 1.33 with SD 0.52. The mean difference was high and statistically significant in experimental group.
In the control group, the pretest mean score was 2.46 with SD 0.52 and post test score was 1.83 with SD 0.45. The mean difference was high and statistically significant. This due to the normal treatment.
To associate the pretest level of respiratory signs part I and part II in preschooler with selected demographical variables (include age, sex, education, patent education, parent occupation, family monthly income, chief complaints to respiratory signs, duration of hospitalization, and area, pet animals in house, type of allergy) in experimental group and control group.
There is no association between the pretest level of part-I respiratory signs among the preschooler with their selected demographic variables like sex, parents education, parents occupation, family monthly income, area of living, type of allergy except age, education, chief complaints to respiratory signs, duration of hospitalization, pet animals in house in experimental group and control group.
There is no association between the pretest level of part-II respiratory signs among the preschooler with their selected demographic variables like sex, parents education, parents occupation, family income, area of living, type of allergy excepts age, education, chief complaints to respiratory signs, duration of hospitalization, pet animals in house in experimental group and control group.
Assess the effect of strelinikova breathing exercise on reduction of respiratory signs on comparing to posttest of both groups (Strelinikova breathing exercise, n.d).
In part I in the experimental group the pretest mean respiratory signs score 6.06 with SD 1.66 and in the control group the mean score was 5.86 with SD 1.60. The mean difference was low and statistically not significant. That is both groups are equal in the pretest level of respiratory signs. So they are comparable.
In the experimental group, posttest mean respiratory signs score was 3.66 with SD 0.72 and in the control group was 4.93 with SD 1.27. The mean difference was high and statistically significant. That is the Strelinikova breathing exercise was effective in part I respiratory signs.
In part II in the experimental group the pretest mean respiratory signs score 2.60 with SD 0.51 and in the control group the mean score was 2.46 with SD 0.52. The mean difference was low and statistically not significant. That is both groups are equal in the pretest level of respiratory signs. So they are comparable.
In the experimental group, posttest mean respiratory signs score was 1.33 with SD 0.52 and in the control group was 1.83 with SD 0.45. The mean difference was high and statistically significant. That is the Strelinikova breathing exercise was effective in part II respiratory signs.
The following conclusion were drawn from the study
The study has several implications for the following fields.
Nurse administrator can include in the polices regarding breathing exercise to prevent respiratory infection in the routine care.
I would like to thank my Principal Dr. Mrs. Santhi Appavu (Ph.D (N)), Christian College of Nursing, Neyyoor for her tremendous effort and who has helped me to the midst of her terrific administrative responsibilities. I thank my guide Mrs. F. Malchijah Ramesh, HOD, Child Health Nursing, Christian College of Nursing, Neyyoor for her guidance, genuine concern, encouragement, and constructive suggestions throughout this study. My sincere appreciation goes to patients of Agasthiya Muni Child Care Centre for being cooperative during the study.
Conflict of the Study: Nil
Source of Funding: Self