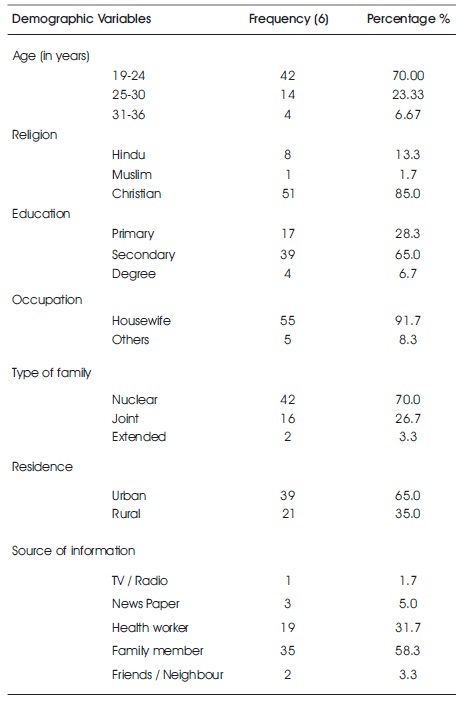
Table 1. Demographic Variables of Samples, N=60
Breast engorgement is a physiological condition during the first two weeks of child birth in which there is lymphatic and vascular congestion and pressure of new milk. It is associated with hard, painful, throbbing, aching, and tender breasts, which may result in women needing analgesia, developing mastitis or temporarily or permanently stopping breastfeeding. The nurse should understand the effect of breast engorgement on the mother and recognize its influence on the baby. One group pre-test - post-test research design was adapted for the study. In view of the nature of the research problem and objectives, a structured questionnaire and structured teaching programme was developed in the initiation of breastfeeding within one hour of birth, composition of breast milk, advantages of breast feeding, techniques and problems of breast of breastfeeding and its management. Sixty primi postnatal mothers were selected by non-probability convenient sampling technique. Structured Knowledge questionnaire was used to collect needed data. After pre-test the structured teaching on prevention and management of breast engorgement was given for 45 minutes. Post-test was administered after five days. The data collected were tabulated and scrutinized by using descriptive and inferential statistics. Results show that 90% of the mothers had an overall inadequate knowledge, 10% of postnatal mothers had moderately adequate knowledge, and none of them had adequate knowledge in pre-test. In post-test 18% had moderately adequate knowledge and 82% of postnatal mothers had adequate knowledge and none of them had inadequate knowledge regarding prevention and management of breast engorgement. The study concludes that the planned teaching programme was effective in improving the knowledge of the postnatal mothers regarding prevention and management of breast engorgement.
Breastfeeding is widely encouraged in current obstetric practice while its advantages to mother and child are well recognized, there are a number of problems associated with it. One common problem that is encountered is breast engorgement, which makes continuation of breast feeding difficult. Breast engorgement occurs if the baby removes less milk from the breast when feeding than the amount that the mother produces. Breast engorgement is the overfilling of breast milk that causes discomfort and pain to the mother whilst non-infectious mastitis is inflammation of the breast due to milk duct blockage (Gillespie, 1995).
Correct breastfeeding technique is important to ensure successful breastfeeding. Incorrect technique may contribute to breast engorgement and in particular it is important for the baby to latch on to the breast correctly during feeding. So that is can suck effectively and in order to do this the baby needs to be correctly positioned, and new mothers may also need advice on this (Ibrahim & Ansari, 2016). Breast engorgement usually occurs within a week of the birth, but can occur later. Primary engorgement occurs in the first few days after the baby is born, and it occurs when the mother's body is still trying to adjust to the amount of milk that the baby demands. Secondary engorgement occurs later when the mother is not feeding as frequently as she used to or the baby removes less milk from the breast (Seda, 2008). Breast engorgement is a painful problem that can lead to premature weaning. It is a common complication of the early puerperium and usually occurs between 3 - 6 days after delivery (Subbiah, 2003). The incidence rate of breast engorgement all over the world is 1: 8000 and in India it is 1: 6500. Engorgement symptoms occur most commonly between 3rd and 5th postnatal day, more than two - thirds of women with tenderness on 5th postnatal day, but some as late as 9th -10th postnatal day. The 20% postnatal mothers especially primigravid mothers are affected with breast engorgement from 0-4 days of postnatal period (Nikodem et al., 1993).
Breast engorgement occurs in 72% to 85% in postnatal mothers. It is a painful unpleasant condition affecting large number of women in the early postpartum. During a time when mothers are coping with demands of the baby it may be particularly distressing. Breast engorgement inhibit the development of successful breastfeeding leading to early breastfeeding cessation, associated with more serious illness including breast infection (Whithley, 2000).
Eapen and Fernandes (2013) had done a study to assess the effectiveness of an information booklet regarding home remedial measures for breast engorgement. An evaluative approach with one group pre-test post-test design was used for the study, forty samples were selected by using simple random sampling technique. Data was collected by using interview schedule to assess the socio demographic data and structured knowledge questionnaire to assess the knowledge regarding home remedies. The collected data were analyzed using descriptive and inferential statistics. A significant difference between pre-test and post-test knowledge was found (t = 14.78, P < 0.05). The study result showed that the information booklet was effective in improving knowledge of the postnatal mothers by providing an information booklet on home remedial measures for breast engorgement (Eapen & Fernandes, 2013).
Chiu et al. (2010) had done a study to compare the effect of Gua-sha therapy and traditional breast care on breast engorgement. A randomized controlled trial was employed to assign participants randomly into intervention (Gua-sha therapy) or control (hot packs and massage) groups. 54 mothers were selected for this study. Data were collected by using interview schedule to assess the socio demographic data and ten point breast engorgement scale was used to assess the breast engorgement. Analysis was done using both descriptive and inferential statistics. Results showed no statistical differences between the two groups at baseline. Body temperature, breast temperature, pain levels, and discomforting levels were statistically different within the two groups at 5 and 30 min after intervention (P < .001). The results of generalized estimating equation analysis indicated that, with the exception of body temperature all variables remained more significant (P < .0001) in improving engorgement symptoms in the experimental group than those in the control group, The findings concluded that Gua-sha therapy had more effective than traditional breast care on breast engorgement (Chiu et al., 2010).
The primi postnatal mothers will have significant improvement in the level of knowledge regarding the prevention and management of breast engorgement after attending the structured - teaching programme.
A quantitative approach with pre-experimental ; one group pre-test – post-test design was adopted for the present study. The sample consisted of 60 primi postnatal mothers in Kanyakumari District by using purposive sampling technique. The researcher used two data collection instruments.
Demographic proforma was used to collect the baseline socio demographic information about the primi postnatal mothers.
A structured – Questionnaire: It consisted of 30 close ended questions to assess the knowledge regarding structured and functions of breast, meaning, causes, signs and symptoms of breast engorgement, basic beliefs of initiation of breast feeding, diagnosis management, and prevention of breast engorgement. Each questionnaire had four options out of which only one option was correct ; The correct answer was given a score of '1' and the wrong answer was scored '0'. The total score was 30.
The content validity of the tool was obtained by submitting it to 10 experts. According to their opinion the tool got its final form. Spearman – Brown method was used to test the reliability of the tool and the value of r = 0.94 revealed that the tool is reliable.
Pilot study was conducted on six primi postnatal mothers to assess the feasibility and practicability. It was considered both feasible and practical. Prior permission for conducting the study was obtained from the concerned authorities. Data were collected only after obtaining the informed consent from the samples. The inclusion criteria for the study were primi postnatal mothers between the age group of 19 - 36 years who are willing to participate in the study. The exclusion criteria for the study were high risk mothers with post partum haemorrhage, septicaemia, and postpartum psychosis.
On the first day of data collection, a pre-test was conducted by using structured questionnaire and assessed the necessity for giving the intervention. The intervention was given in the form of structured teaching program. Post- testing was done to assess the effectiveness of structured teaching programme in terms of improving in knowledge regarding prevention and management of breast engorgement. Data were collected and analyzed using descriptive and inferential statistics.
Data presented in Table 1 showed that the majority of 42 (70%) samples were in the age group of 19 - 24 years, 51 (85%) were Christian, 37 (61.7%) had secondary education, 55 (91.7%) samples are housewives, 42(70%) belong to a nuclear family, 39 (65%) of samples are residing in an urban area, and 35 (58.3%) of samples acquired information from the family members regarding prevention and management of breast engorgement.
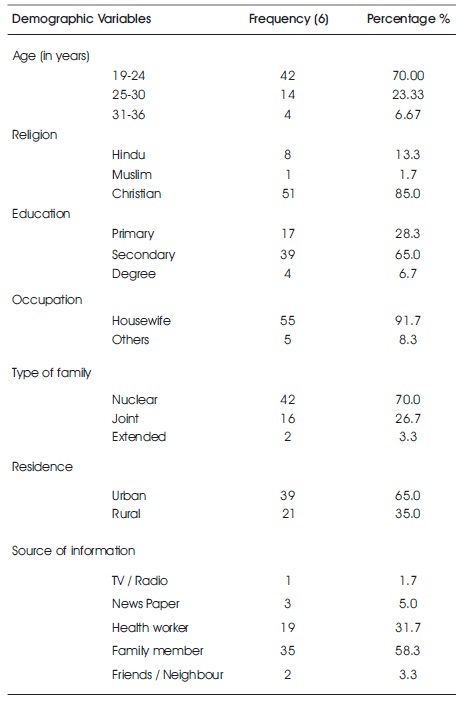
Table 1. Demographic Variables of Samples, N=60
Table 2 shows the mean knowledge score was 7.80 in pre-test and 27.88 in post-test. The calculated “t” value 12.63 was greater than the table value of 1.96 at a significance level of 0.05 level. The difference between pre-test and post-test was statistically significant at 0.000 level, which indicates that structured teaching programme was effective in improving the knowledge about prevention and management of breast engorgement in postnatal mothers.
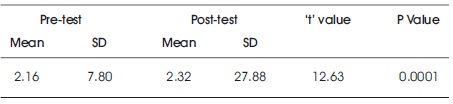
Table 2. Mean, Standard Deviation, Paired 't' Value and P Value of the Pre-test and Post-test Knowledge Score
Malathi (2008) conducted a pre-experimental study to determine the effectiveness of planned teaching programme on breastfeeding problems among primi gravida postnatal mothers and its management. This study included the problems like mastitis, breast engorgement, flat nipple, and sore nipples. The study revealed that planned teaching programme was effective in improving the knowledge of the mothers.
The findings of the study showed that the mean changes between pre-test and post-test score was found to be highly significant and there was a significant association between the pre-test knowledge level and selected demographic variables like age, education, occupation, and source of information for knowledge at 0.05 level. Hence, the administration of STP was effective in improving the knowledge level of prevention and care of breast engorgement among primi postnatal mothers.
The findings of the study have considerable implications on Nursing practice, Nursing Education, Nursing Administration, and Nursing Research.
The present study assessed the knowledge among primi postnatal mothers regarding prevention and management of breast engorgement. The study found that the primi postnatal mothers had inadequate knowledge regarding prevention and management of breast engorgement. After the structured teaching programme on prevention and management of breast engorgement, there was a significant improvement on knowledge of the primi postnatal mothers regarding prevention and management of breast engorgement. The study concluded that the structured teaching programme was effective in improving the knowledge of primi postnatal mothers regarding prevention and management of breast engorgement.