Preceptorship is a one-to-one relationship of predetermined length between an expert nurse and a nursing student. During the preceptorship, student nurse learns the roles and responsibilities of clinical nursing in a particular area of practice. The preceptorship model is designed to assist the student in successfully adjusting to and performing his/her new role. This is a student centered approach which assists students in becoming more deeply engaged in patient care by providing more hands on care.
The preceptor, preceptee and the faculty plays an important part in student's learning and contribute towards role transition. Therefore, it is essential that all three of them work in collaboration, extend their support and have well developed understanding to make the experience meaningful. In this paper to follow, the author discuss the background and significance of preceptorship and its application in clinical practice, integrating the Synergy model of preceptorship for learning and care. Later in the paper, the author discuss the roles and functions of the preceptor, challenges, training needs, and the benefits of preceptorship model at the organization level.
Newton, Cross, White, Ockerby, Billett (2011) mention in one of their article about the growing criticism for the newly graduate nurses as not “work ready” i.e. these newly graduate nurses do not perform according to the expectations of the healthcare organizations. This has lead to decreased productivity and has imposed large costs to the healthcare institutions. Hickey (2009) indicates a study carried out to identify preceptors' views of new graduates' readiness for practice using a specific set of criteria which revealed lacking in certain areas of clinical practice. These included psychomotor skills, assessment skills, critical thinking, time management, communication skills and teamwork. Moreover, according to the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), inadequate orientation and training of nurses contribute to 58% of serious errors in clinical settings (Baggot, Hensinger, Parry, Valdes & Zaim, 2005). Based on these literature findings, it is essential to train nursing students and expose them to the clinical learning environment such that when they enter into the real world of nursing, they are at ease to practice. According to Hayes and Harrell (1994) the word preceptor has been known since the 15th century in England and since the 1960 the concept of preceptorship has been explored and used in the literature of nursing service administration and education. Literature review reveals that preceptorship model is not only used in nursing education, but also in Pharmacy, medicine and dentistry to train students in their respective fields (Billay & Yonge, 2004; Billay & Myrick, 2008).
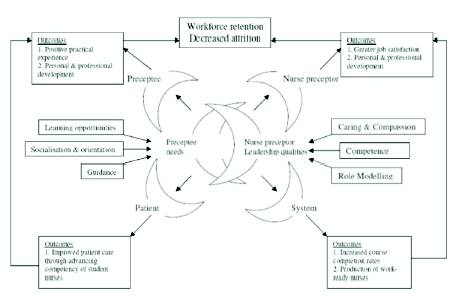
The purpose of this synergy model of preceptorship here is to have a better understanding of the relationship between preceptor, preceptee, the healthcare system and the patient. According to Zilembo and Monterosso (2008) originally the synergy model was proposed by Curley in 1998 as a patient care model. Later this model was adapted and implemented in a variety of clinical settings by different researchers. Alspach (2006) included the element of preceptorship in the synergy model based on optimum orientation to meet the needs of nursing students through preceptor competencies. All these researchers considered “patient care, leadership and nursing preceptorship as interrelated elements that contribute to the learner's clinical experience” (Zilembo & Monterosso, 2008, p.90).
The adaptation of the synergy model by Zilembo & Monterosso (2008) as Proposed Synergy Model of Preceptorship for Learning and Care (appendix A) revolves around preceptee's experience of positive clinical practice based on preceptor's demonstration of certain leadership characteristics. Moreover, the model links the four basic elements of leadership, preceptorship, learning, and the learning environment considering leadership as a unique phenomenon defined in its context. The underlying principle of the model also highlights the importance of variance due to individuality of personality and circumstances. The model suggests that nurse preceptors who display leadership characteristics such as (caring and compassion, competence and role modeling) enhances student's (preceptee) needs of the clinical experience such as (learning opportunities, socialization, orientation and guidance) resulting in positive personal and professional outcomes for both the preceptee and preceptor. These outcomes later lead to improved patient care and satisfaction through the competency of the student nurse; as well as positively benefit the organization (system) in terms of production of work- ready nurses and timely completion of the course. Finally, the organizational outcomes result in nurse preceptor's job satisfaction and professional development which leads to workforce retention and decreased attrition. The patient related outcomes reward the student (preceptee) with positive practical experience and personal and professional development, decreasing the reality shock and providing a smooth transition.
Lastly, in support of the synergy model of preceptorship, Happel (2009) states that “the success of the preceptorship is determined by the strength of the relationship between the student (preceptee) and the professional (preceptor)” (p. 373). The important concepts from the Synergy model of preceptorship are discussed further in this paper.
The selection of preceptors is critical to the success of the preceptorship program. The importance of preceptorship program is well explained in the light of evidences. As it is well known that preceptor plays a key role in the preceptorship experience, therefore it is vital to choose those nurses for this position who are willing to commit and accept this heavy responsibility and work sincerely. Speers, Strzyzewski and Ziolkowski (2004) mention the selection criteria which should be taken into account when choosing the preceptors. This criterion includes the preceptor's experience in the nursing field, decision making ability of the nurse, expertise in the use of various resources and working in stressful environment, ability to provide quick and relevant feedback, demonstrate professional attributes, teaching skills and leadership qualities, able to promote positive and confidential interpersonal relationships, and is willing to be a preceptor.
Along with the above mentioned selection criteria, it is important that the preceptor should possess leadership qualities and is vigilant enough to promote learning and develop critical thinking skills in the students. The preceptors are required to give daily feedback on the preceptee’s performance and evaluate them accordingly. This is an important skill that has to be learnt and mastered. Role model, educator, evaluator, socializing students and protector are some of the leadership roles played by a preceptor. Along with these, different studies have reported genuine concern for the preceptee, excellent communication skills, a positive attitude towards learning and teaching and professional growth of nursing students as added qualities of a good preceptor (Speers, Strzyzewski & Ziolkowski, 2004; Barker & Pittman, 2010; Zilembo & Monterosso, 2008). Preceptors should be given training in this case so as to learn how to give critical feedback while maintaining the student's integrity and self-respect.
Barker and Pittman (2010) have reported the impact of preceptor's efforts on the student's formation and described ways in which the preceptor's distinctive position influences the ways in which the student forms a basic framework for practice. Identifying adequate number of clinical preceptors in this era of nursing shortage is itself the biggest challenge. Along with it, the preceptors have a higher responsibility of guiding the preceptee towards the right track. It is sometimes very difficult for the preceptors to embrace extra time out of an already packed schedule to guide their preceptees. Duteau (2012) believes that “the time and energy required providing effective precepting through monitoring and teaching greatly adds to the pressure on the overburdened and overworked nurse” (p. 39). The preceptors are expected to fulfill the objectives of the students, overcome such challenges of time constrains and the work load. These challenges demand the preceptor to be vigilant enough to identify the student's learning needs and patient encounters to meet those needs and adjust them into the available time constraints (Barker & Pittman, 2010). According to Giallonardo,Wong and Iwasiw (2010) “preceptors are expected to be role models, nurturing, compassionate and experts in clinical knowledge” (p. 995). Moreover, preceptors are obliged to maintain the level of efficiency that existed before the preceptorship and assure that all regulations and policies are followed. In addition to these challenges, lack of support from peers, lack of time spent with the student and nursing faculty are also reported by Duteau (2012).
The synergy model of preceptorship suggests that successful preceptor- preceptee relationship results in greater job satisfaction among preceptees along with personal and professional development (Zilembo & Monterosso, 2008). Despite such challenges, enhanced sense of responsibility and an opportunity to demonstrate clinical competency and teaching ability are reported as intrinsic benefits of preceptorship by many researchers (Barker, 2010; Lee, Tzeng, Lin, & Yeh, 2009; Billay & Yonge 2004). Research suggests that a powerful influence on the decision of being a preceptor is “personal satisfaction and a desire to ''give back'' to the students to repay those who invested in their education” (Barker & Pittman, 2010, p.145). In addition to internal motivation, preceptors have reported that their decision to precept was based on their own experience of being preceptored. Hyrkas and Shoemaker (2007) suggest that preceptorship provides preceptors an opportunity for self-learning, creates a feeling of value to their organization, enrichment of leadership skills and more commitment towards their job responsibilities. Along with these, extrinsic benefits reported in the literature include letters of appreciation, education credentials, and opportunities to attend conferences.
Duteau (2012) reveals that 35% to 65% new Canadian nursing graduates leave their job within the first year which contributes to a 55% of turnover rate. The results are thought provoking for the leaders. There is a serious need to improve or design strategies to ensure effective orientation and socialization of new nurses. Willemsen-McBride (2010) found preceptorship planning as an essential component in retention of nurses and concluded that proper preceptor- student learning style as one of the ways of enhancing job satisfaction level. Lee et al. (2009) also reported the significant drop of 46.5% turnover rate than the previous year, after the introduction of a preceptoship program. In addition to these studies, the synergy model of preceptorship also supports that the collaboration between preceptor and the preceptee results in earlier course completion for the student and therefore availability of work- ready nurses. The foreseen benefit to the organization would be workforce retention and decrease attrition.
To sum up, preceptorship has been recognized by researchers as crucial strategy to assist in the mastering of skills and knowledge, enhance confidence and socialize students into the expectations of the profession and enhance recruitment into the nursing profession. Preceptors should not expect students to be fully skilled and competent at their arrival into the clinical learning environment. Mamchur and Myrick (2003) believe that poor clinical experience can result in student disappointment about nursing and an inability to integrate and learn. Therefore, it is important for all those affecting the preceptor- preceptee relationship including the nursing faculty, nursing school and the healthcare organization and nursing managers to try their utmost to create such an environment that fosters students' learning and at the same time build a positive picture of the workplace environment. The value of a preceptor is such that they are referred to as “the last quality control measure to ensure those nurses who are about to enter the professional work environment are competent to do so” (Earle-foley, myrick, luhanga & yonge, 2012, p. 30). It is evident that with all the challenges to the nursing profession, with nurse shortages, where the nurses take care of more patients than ever, have high levels of responsibility, and represent varying levels of education and experience, Yet, preceptorship model is a success and contributes to effective clinical learning and facilitates the role transition for the undergraduate students. Since the preceptor role is critical to the development and retention of an adequate nursing workforce, the transition to independent practice also influences effective staffing, turnover, and retention at the unit level and within the institution, as well as job satisfaction. Thus, effective preceptor-preceptee relationship and willingness to learn can earn fruitful results.