Table 1. Socio Demographic Profile of Study Subjects (N=60)
Cardiac catheterization remains the gold standard diagnostic test and evaluation for coronary heart diseases. The aim of this study was to investigate the effect of low fowler's position (30o) on the severity of back pain and local vascular complications following transfemoral cardiac catheterization. A Randomized Controlled Trial (RCT) is the design principle used here. The study was conducted in the Advanced Cardiac Centre of Post Graduate Institute of Medical Education and Research, Chandigarh, India. A total 60 patients scheduled for elective transfemoral diagnostic cardiac catheterization were included in the study. Patients were randomly assigned to the control group (n=30) and the experimental group (n=30). Data were collected through the self developed 'Interview schedule, 'Numerical pain intensity scale', and 'Vascular complications assessment' tools after checking its validity and reliability. Low fowler's position protocol and the protocol for assessing vascular complications were also developed. Both groups were restricted to bed rest for first 2 hours following the procedure in supine position with the affected leg straight and immobilized. After 2 hours, patients in the control group (n=30) were receiving conventional care in supine position and patients of the experimental group (n=30) were restricted to bed rest in low fowler's position with the head of the bed elevated to 30 degree. Severity of back pain was assessed at regular time intervals of 2, 4, 6 hours of post cardiac catheterization. Local vascular complications (hematoma, ecchymosis, and bleeding) were assessed at the time of removal of dressing at 12 hours after catheterization. The experimental group patients significantly had less back pain than the control group (p<0.01) at 4 hours and 6 hours after cardiac catheterization. The control group patients (on supine position) significantly developed ecchymosis as compared to the experimental group (on low fowler position) (p<0.02) at the time of removal of dressing from the puncture site. None of the patient developed hematoma in both groups. There was no major bleeding in any of the groups. Nursing patients in low fowler's position at 30 degree during the early hours after cardiac catheterization can minimize the severity of back pain and ecchymosis.
Coronary artery disease is one of the leading causes of death in the world. Cardiac catheterization is the gold standard diagnostic test for coronary heart diseases (Keeling AW, et al., 1996). Although it can be performed through brachial, radial or femoral arteries, most (>95%) cardiac catheterizations are performed through the percutaneous femoral technique (Chair et al., 2007) .
This invasive procedure is not entirely free from the risk of complications (West R, et al., 2006). Vascular complications such as bleeding, hematoma, and ecchymosis are the most common complications after cardiac catheterization that could be resulted from a trauma to the femoral artery (Chair SY et al., 2003 & Steffenino G et al., 2006).
Due to the potential vascular complications, all patients are restricted to bed rest in the supine (flat) position with the affected leg immobilized for 6-24 hours after the procedure, to prevent bleeding from the insertion site, which usually occurs in 0.43 - 4% of patients (Benson G, 2004; Chair SY, et al., 2003;). Conventional care after cardiac catheterization involving the femoral artery site routinely include supine (flat) bed rest for 6 - 24 hours, to prevent vascular complication of the insertion site. Bearing such a prolonged bed rest in the supine position, is difficult for many patients, and is often associated with discomfort, especially back pain (Winslow HE, 1996; Fowlow B, et al, 1995). Studies show that back pain is frequently pronounced by the flat supine position without hip flexion (Lunden MH, et al., 2006).
Pain leads to many harmful effects by activating the biological stress response. As a result, the autonomic nervous system is activated and releases the epinephrine. It increases heart rate and blood pressure and consequently brings about an increase in myocardial workload and oxygen consumption, both of which can cause or exacerbate myocardial is chemia and even infarction in vulnerable patients (Dumont CJ, et al., 2006).
It is noteworthy that this recommendation for prolonged bed rest in the supine position is based on tradition rather than on research (Roebuck A, et al., 2000; McCabe PJ, et al., 2001). Studies have shown that modified positioning can reduce back pain without any statistically significant increase in the incidence of post catheterization complications (Chair SY, et al., 2007; Chair SY, et al., 2003; Fowlow B, et al., 1995). Hence an attempt has been made to assess the effect of low fowler position after cardiac catheterization.
The main objective of the present study is to investigate the ° effect of low fowler's position (30 ) on the severity of back pain and local vascular complications following transfemoral cardiac catheterization.
There will be no significant difference between supine and the low fowler position on post transfemoral diagnostic cardiac catheterization on the patient's outcome in terms of severity of back pain, and local vascular complication like bleeding, hematoma, and ecchymosis at the 95% level of confidence.
A two group Randomized Controlled Trial (RCT) design was adopted in the present study with an intention to evaluate the effect of low fowler position after cardiac catheterization in terms of back pain and local vascular complications.
The study was conducted in the cardiothoracic units of the Advanced Cardiac Centre of a referral hospital in north India during the year 2011-12. This hospital is functioning as a tertiary level care hospital to cater the needs of northern India. Over 1400 beds with super specialty clinical facility house were available for patients with varying degree of illnesses.
The target population included all the elective patients (83 patients) undergoing elective transfemoral diagnostic cardiac catheterization with 6F catheter size. Out of 83, 21 were excluded as per the criteria and 2 subjects are declined to participate and 60 subjects were finally enrolled in the study. A sample of 60 were assigned to the control group (n = 30) and the experimental group (n = 30) by a simple random method using non-replacement lottery method. The control group patients were on complete bed rest for 6 hours on lying supine position after cardiac catheterization; the experiment group patients were placed on low fowler position (30 degree) as per the developed protocol on complete bed rest for 6 hours after cardiac catheterization.
The data were collected by using assessment, interviewing and observation methods. The tools used for data collection were interview schedule, numerical pain intensity scale, vascular complication assessment tool, and record proforma.
The interview schedule was developed to gather information regarding socioeconomic, demographic profile of the subjects, a brief personal history, clinical profile, and the details of cardiac catheterization.
A numeric pain intensity scale was used to assess the level of back pain intensity. It is a standardized tool introduced by the National Initiative on Pin ControlTM (Loaville et al, 2003), represented on a 100 mm long line showing 0 to 10 scores (0 score: no pain, 1-3: mild pain, 4-6: moderate pain, and 7-10: severe pain).
A vascular complication assessment tool was developed to assess hematoma, ecchymosis and bleeding in or around the catheter puncture site on an ordinal scale, 0 to 4 on the basis of categories. The bleeding was categorized as major (bleeding causing hemodynamic instability or requiring transfusion), minor (bleeding requiring compression without any hemodynamic instability) and no bleeding
Hematoma was assessed as grade 0 (Benign: No bleeding, no hematoma), Grade 1 (Small hematoma, scanty oozing, no intervention except application of 4×4 gauze), Grade 2 (moderate hematoma or bleeding: application of manual pressure for ≤ 15 minutes), Grade 3 (Large hematoma of > 5 cm or bleeding: extended pressure application for > 15 minutes), and Grade 4 (Surgical intervention, hematoma evacuation).
Ecchymosis was measured from grade 0 to grade 4 (Grade 0: No ecchymosis, Grade 1: ≤ 2 cm, Grade 2: >2 cm but ≤ 3cm, Grade 3: >3 cm but ≤ 5 cm, Grade 4: >5 cm). Hematoma and ecchymosis was measured by using a two dimensional ruler with the precision of 1 cm2 . A proforma was designed to record back pain, heart rate, blood pressure at different time intervals of 2, 4, and 6 hours following catheterization. A protocol for ‘Low fowler’ position was developed.
The research tools & protocol on a low fowler position were checked for its validity by different experts of medical and nursing field and found valid. Reliability of numerical pain intensity scale and vascular complication assessment tool was determined by inter-rater agreement using Cohen's Kappa with 95% confidence interval. The value of items varied from 0.88 - 0.91, which indicated that the tools were reliable. A pilot study on 10 subjects was undertaken and the feasibility of the study was found.
Ethical approval for the study was obtained by the institutional Ethical Committee. A written permission was obtained from the head of Cardiac Department. Sister-incharge of the respective units was informed about the study. The subjects were explained about the aim, benefits and possible hazards of the study; a written consent was obtained from them. The anonymity and confidentiality of the participants in relation to the findings were protected while reporting the study.
The subjects' socio-demographic, clinical data were collected. Subjects of both groups were kept in a supine position for 2 hours after cardiac catheterization. The subjects of the control group received routine care and were in the supine position till the removal of the dressing; and the subjects of the experimental group were placed in ° low fowler's position (30 ) after 2 hours of catheterization. Both groups were assessed at 2 hours (base line), 4 hours and 6 hours of post catheterization for heart rate, systolic and diastolic blood pressure and for pain intensity. The assessment for the presence of local vascular complications: hematoma, ecchymosis and bleeding were made at 12 hours at the time of removal of dressing. Thus the main outcomes used in this study are back pain intensity, hematoma, ecchymosis, and bleeding.
The data were analyzed using both descriptive and inferential statistics with the help of Microsoft Excel (2007) and Statistical Package for Social Science (SPSS) programme version 16. Socio-demographic data were analysed in terms of frequency and percentage for categorizing data and the means and standard deviation of the interval data. The chi square and independent ‘t’ test were used to compare both the experimental and control groups for its homogeneity, and vascular complications; whereas independent ‘t’ test & a repeated measure ANOVA with Greenhouse-Geisser correction was used to compare the severity of pain
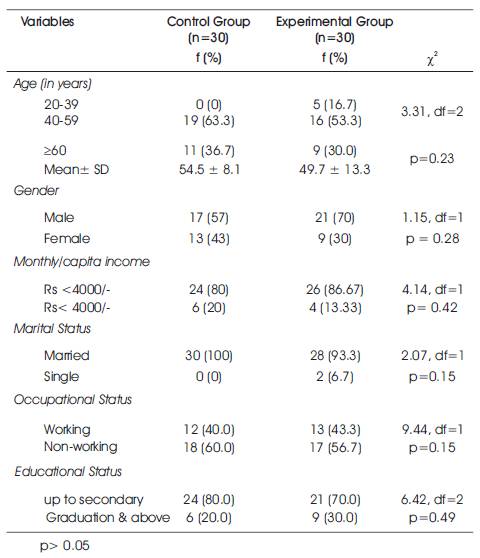
More than half of the subjects in both groups i.e. 19 (63.3%) in the control group and 16 (53.3%) in the experimental group were between 41 to 60 years of age. The mean age of subjects in the control group and the experimental group were 54.5 ± 8.1 and 49.7 ± 13.3 years respectively. It ranged from 40-70 years in the control group and 20-70 years in the experimental group. More than half of the subjects in control group 17 (56.7%) and experimental group 21 (70%) were males. The majority of subjects in both the groups i.e. 24 (80%) subjects in control group and 26 (86.67%) subjects in the experimental group were having per capita monthly income < Rs 4000/-. The majority of the subjects in both groups was married and qualified up to secondary education. Both groups were comparable as per their age, gender, religion, occupation, income, and educational status (p> 0.05) as shown in Table 1.
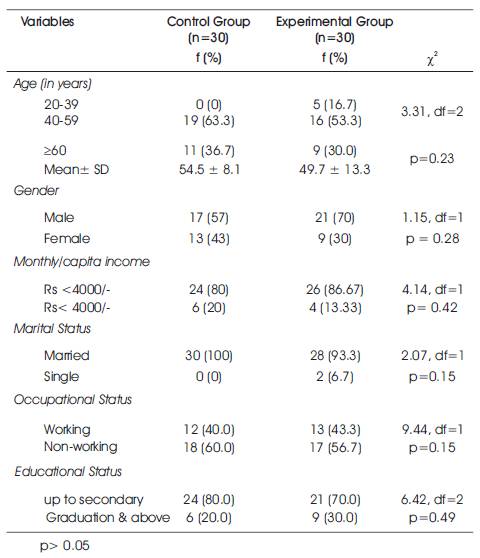
Table 1. Socio Demographic Profile of Study Subjects (N=60)
The data revealed that out of 30 subjects in each group, 12 (40%) subjects from the control group and 13 (43.3%) subjects from the experimental group had a history of hypertension. Fourteen (46.7%) subjects from the control group and 21 (70%) subjects from experimental group was having a history of cardiac disease. 14 (46.7%) subjects from each group were using antithrombotic (clopidogrel, ecospirin). Majority of the subjects in both groups i.e. 26 (86.7%) subjects in control group and 22 (80%) subjects from experimental group had no history of previous cardiac catheterization. Mean Body Mass Index (BMI) in the control group and the experimental group was 23.54 ± 3.51 and 23.29 ± 3.99 kg/m2 respectively. Both groups were comparable in terms of their history of hypertension, cardiac disease, previous cardiac catheterization, Body Mass Index, diagnosis as shown in Table 2, and preprocedural coagulation profile (p> 0.05) is concerned.
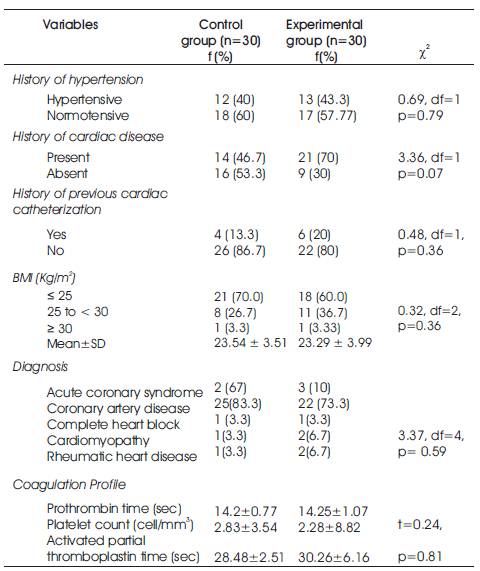
Table 2. Clinical Profile of Study Subjects (N=60)
30 patients in the experiment group, during pre intervention period at 2 hour of catheterization, 19 (63.3%) had no pain, 10 (33.4%) had mild pain, 1 (3.33%) had moderate pain and none had severe pain and after intervention at 4 hours after catheterization, 18 (60%) patients did not experienced back pain, 11 (36.6%) had moderate pain, and none had severe pain; at 6 hours after catheterization, 23 (76.6%) experienced no back pain, 7 (23.3%) experienced mild pain, and none of the patient experienced either moderate or severe pain. Of 30 patients in the control group 15 (50%) experienced no pain, 12 (40%) mild, 3 (10%) moderate pain and none experienced pain at 2 hours after catheterization; at 4 hours after catheterization, 3 (10%) had no pain, 21(69.9%) had mild, and 6 (20%) had moderate pain; at 6 hours after catheterization, 1 (3.33%) had no pain, 12 (40%) had mild, 14 (46.5%) had moderate and 3 (10%) experienced severe back pain as shown in Figure 1.
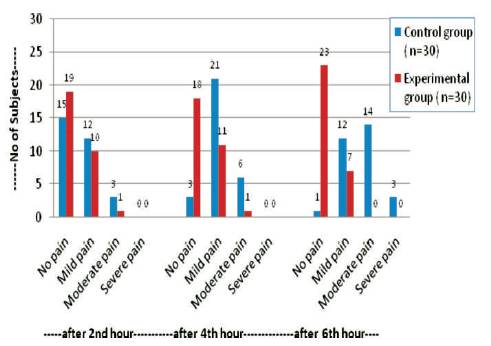
Figure 1. Severity of Back Pain among Subjects
The data also revealed that at two hours after cardiac catheterization (at baseline), statistically there was no significant difference in the mean back pain scores in both groups, (p=0.23). But at four and six hours after the catheterization, the experimental group patients had significantly less back pain scores than the control group (p<0.01). In the experimental group (with low fowler position), the back pain was significantly reduced from two hours to 6 hours (F=5.29, p<0.01), and in the control group patients (with supine position), the back pain significantly increased from two hours to 6 hours after cardiac catheterization (F=83.51, p<0.01) and is shown in Table 3 & Figure 2.
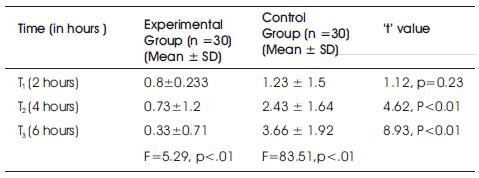
Table 3. Back Pain Score among the Experimental and Control Group Patients at different Time Interval after Cardiac Catheterization
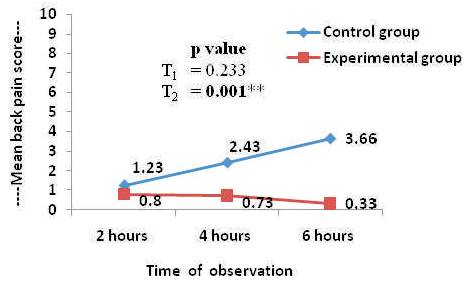
Figure 2. Severity of Back Pain at Different time Intervals among Control and Experimental Group
While assessing the patients' outcomes in terms of vascular complications such as hematoma, ecchymosis and bleeding at the 12 hour of post cardiac catheterization, none of the patients in both the groups developed hematoma at the puncture site or had major bleeding. Only one patient in the experimental group had minor bleeding, but statistically no significant difference was observed in both the groups (χ2=1.02, p=0.31). The ecchymosis was found significantly less in the experiment group (low fowler's position) than in the control group patients (supine position) (χ2=9.31, p=0.02). More than 85% patients in the experiment group had no ecchymosis as compared to the control group (53.3%).
Cardiac catheterization is widely used for the diagnostic evaluation among patients with cardiac diseases (Woods SL, et al., 2005). Despite progressive improvements in non invasive techniques, it remains the gold standard for the assessment of anatomy and physiology of the heart and its associated vasculature (Kasper DL, et al., 2005). More than 95% cardiac catheterization is performed through percutaneous femoral route and this invasive procedure is not free from the risk of complications. The patients are restricted to bed rest and usually kept in a supine position with the affected leg immobilized for 6-24 hours after catheterization to prevent various vascular complications such as bleeding, hematoma formation, and ecchymosis resulted from a trauma to the femoral artery.
Studies reported that this type of position is based on tradition and on empirical reasoning rather than based on evidence and is associated with discomfort and back pain. The present Randomized Controlled Trial is an attempt to evaluate the effect of low fowler's position on the severity of back pain and local vascular complications after transfemoral cardiac catheterization. Both the experimental and control groups were comparable in terms of their socioeconomic, clinical and pre coagulation profile. Both groups were restricted to bed rest with supine for the first 2 hours after catheterization and were comparable in regard to severity of back pain.
The majority of patients in the experimental group placed in a low fowler position after 2 hours of cardiac catheterization experienced a marked reduction in the back pain intensity (Figure 1) and also the average pain scores have significantly decreased from 0.8 ± 0.23 to 0.33 ± 0.71(F=5.29, p=.001) within 6 hours. Whereas the majority of patients in the control group receiving conventional care with supine position experienced a marked increase in back pain and also average pain scores have significantly increased from 1.23 ± 1.5 to 3.66 ± 1.92 (F=83.51, p=.001) within 6 hours (Table 3 & Figure 2). This means that the positioning patient after catheterization has a direct effect on the severity of back pain. Patients positioned in the supine position for six hours in bed, experienced higher severity of back pain as compared to patients positioned in a low fowler position after cardiac catheterization.
A Randomized Controlled Trial conducted by Yilmaz, E, et al., (2007) reported that back pain has been more often in the patients whose position was not changed and whose beds were not raised about 30 to 45 degrees after the procedure (p<.05). The modified position reduces pressure of the bed on tissues and back muscles as compared to lying in a flat position reported by Pooler- Lunse, et al., (1996). Changing position is also associated with an increased comfort and decreased level of fatigue (Chair SY, et al., 2004; Rezaei- Adaryani R, et al., 2009a and less pain intensity by positioning the patients at 45o in a fowler position (Pooler-Lunse, et al.,1996;); in fowler's position in different angles every two hours experienced less pain at 3, 6, 8 hours (Rezaei-Adaryani R, et al., 2009b); or intermittently changing to 15o , 30o , 45o after cardiac catheterization is also reported as compared to the control group placed in the supine position (Sabzaligol M, et al., 2008).
In the present study low fowler positioning after cardiac catheterization was found more effective in reducing the ecchymosis as compared with a control group receiving a conventional care in the supine position for 12 hours of cardiac catheterization as shown in Table 4. Studies conducted with the fowler position raising head end in different angles found no association of hematoma and bleeding incidence with the positioning patients (supine or fowler position) after cardiac catheterization (Chair et al., 2007; McCabe et al., 2001; Logemann et al., 1999; Botti et al., 1998). In the present study also, none of the patients in both the groups developed hematoma or had major bleeding at the femoral puncture site. However, one patient in the experimental group had minor bleeding at the insertion site on the removal of dressing after 12 hours of cardiac catheterization.
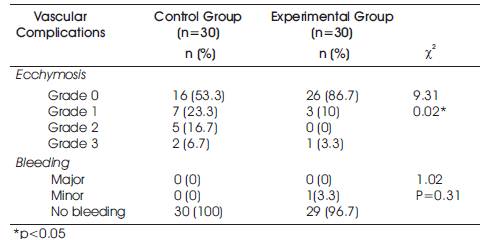
Table 4: Vascular complications Among Experimental and Control Groups at the time of Removal of Dressing (at 12 hours) after Cardiac Catheterization
The findings were in contrast with the studies conducted by Yilmaz E, et al., (2007) reported that, active bleeding was observed among 1.4% cases, minor hematoma in 5.7% cases, and ecchymosis in 15.7% cases whose positions were changed. A retrospective study by McCabe et al., (2001) reported 11.4% patients developing vascular complications with the application of 3-4 hours bed rest and raising the head of the bed at 30 degrees. Babu SC, et al., (1989) reported complication rates in 5,850 patients and out of which 0.23% patients required surgical interventions. Machleder et al (1972) reported vascular complications among 24% and Brener & Couch (1973) reported the same in 28% patients after transfemoral cardiac catheterization. Thus the present study shows that low fowler position (30o) is equally safe in terms of occurrence of hematoma and bleeding and effective in reducing the ecchymosis as compared to the supine position of the restricted patients for 12 hours in the bed after transfemoral cardiac catheterization.
Modified low fowler's positioning protocol has beneficial effects on the patient's outcome, particularly in reducing back pain without the incidence of local vascular complications such as hematoma, bleeding and ecchymosis.
In the light of the findings of the present study, it is suggested that the institutional standard of supine position of bed rest after diagnostic cardiac catheterization via the femoral artery could be safely changed to low fowler's position. Low fowler's position may add to the patient's comfort with reduced severity of back pain without increasing the rate of vascular complications. The study can be replicated in the same setting with large sample and further studies can be conducted to evaluate the effects of different modified positions after transfemoral cardiac catheterization.