Figure 1. System architecture of a wireless M2M healthcare system
This paper presents the development of a personal Machine to Machine healthcare system that is both flexible and scalable. Based on the IPv6 protocol, the system can be used over a low power wireless personal area network. Since a hierarchical network structure offers excellent accessibility, the system is applicable to both local and International healthcare services. To further enhance scalability and reliability, the proposed system combines low power wireless personal area network with mobile techniques, depending on whether the sensor is located inside or outside the range of a wireless sensor network. Employing wearable low power sensors, the system measures health parameters dynamically. For wireless transmission, these sensors are connected to a machine to machine node either through the internet or through an external IPv4/IPv6 enabled network. The low power wireless personal area network protocols to wide area networks were verified in practical tests using a machine to machine gateway. To assess the physical health of an individual, the system uses heart rate variability analysis in time and frequency domain. Acquired data are first stored on a server for analysis. Result of the analysis is then automatically sent to Android based mobile devices carried by the individual or appointed healthcare providers. In this way, mobile techniques are used to support remote health monitoring services. This personal machine to machine healthcare system has the capacity to accurately process large amount of biomedical signals. Moreover, due to its ability to use mobile technology, the system allows the patient to conveniently monitor their own health status, regardless of location.
Healthcare is moving from an approach based on the reactive responses to acute conditions to a proactive approach characterized by early detection, prevention, and long-term management of health conditions. The current trend places an emphasis on the monitoring of health conditions and the management of wellness as significant contributors to individual healthcare and wellbeing, thereby improving the quality of life. The biomedical signals are critical for the advancement of diagnosis as well as treatment of cardiovascular diseases by using wireless wearable sensors [1]–[3]. For example, continuous recording of an Electrocardiogram (ECG) or Photoplethysmogram (PPG) by a wearable sensor can provide a realistic view of the heart condition of a patient during normal daily routines, and can help detect conditions such as high blood pressure, stress [4], anxiety, diabetes, and depression [5], [6]. In addition, it is conceivable that, further automated analysis of recorded biomedical signals could support doctors in their daily practices and allow the development of warning systems. This would bring several benefits: it would increase the health observability, collaboration among doctors, and doctor-to-patient efficiency [7], and thereby decrease healthcare costs. Moreover, such continuous monitoring would increase early detection of abnormal health conditions and diseases, and therefore provide a great potential to improve the quality of life of patients[8]. Recent technological advances in M2M systems together with the rise of M2M communications over wired and wireless links allow the design of lightweight, low-power sensors at low cost for wearable sensor networks, integrated circuits, and wireless communication [9], [10]. At its inception, the future of M2M communication was i-manager’s uncertain at that time, engineers were just beginning to learn how to directly connect cellular technology to other computer systems. However, with the dramatic penetration of embedded devices,M2M communications became a dominant communication paradigm in many applications that concentrate on data exchange among machines to make these machines intelligent in a narrow sense and among currently networked applications and services, whose core is the intelligent interaction of machines in a general sense [11], [12]. As a prime benefit of these new strategies, IP based wireless networks have been a catalyst for accelerated innovation in M2M services, as they have assisted in the identification of hidden growth opportunities in M2M services. The evolution of M2M systems began with the development of a wireless sensor network with the help of an IPv6 technique [13]. Advances in M2M networks allow the establishment of wireless sensor networks by the efficient addressing mechanism of Ipv6 over the IEEE 802.15.4 standard to every node to enhance the quality of data transmission and extend healthcare service coverage [14], [15]. .
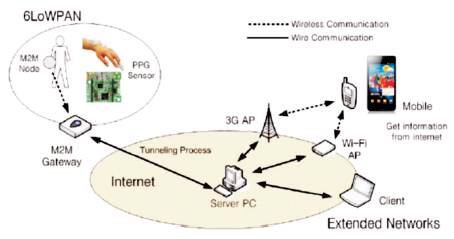
With advances in mobile communication, new opportunities have opened up for the development of healthcare systems that remotely monitor biomedical signals from patients. The availability of a new generation of mobile phones has an important impact on the development of such healthcare systems, as they seamlessly integrate with a wide variety of networks (such as 3G, Bluetooth, wireless LAN, WCDMA and GSM), and thus enable the transmission of recorded biomedical signals to doctors or patients from a central server located in a hospital, home, or office[16]. A smart phone presents a programmable monitoring platform for healthcare as people go about their daily lives [17]. This paper describes a wireless M2M healthcare solution that uses Android mobile devices in a global network which is shown in Figure 1. The use of a global M2M network in healthcare applications promises to replace the use of traditional healthcare systems based on wireless sensor networks, providing ease of measurement, extension of network, accessibility, and reliability. The proposed system also promises to help improve the expansion of healthcare service coverage by providing efficient support for Ipv6.
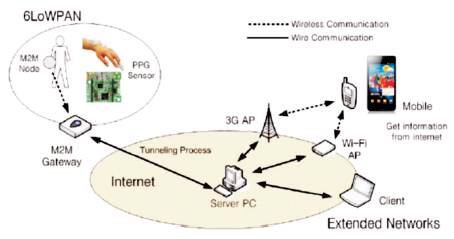
Figure 1. System architecture of a wireless M2M healthcare system
The core hardware devices in the proposed system such as the M2M devices which are designed to measure and transmit the PPG signals in a wireless M2M healthcare system, is shown in Table I. The PPG sensor is designed to obtain the PPG waveforms and oxygen saturation data from a patient's finger by calculating the ratio of red and infrared light on the hardware surface, which depends on the absorption of both types of light. The M2M nodes connected to the wearable sensors are placed on the patient's body and are mainly responsible for collecting and transmitting the sampled signals at 75 Hz for the PPG signals to the M2M gateway. The M2M nodes connected to the wearable sensors are placed on the patient's body in order to collect health parameters such as ECG signals, PPG signals, and an oxygen saturation value and transmit the collected parameters to the server for monitoring and analysis. The M2M gateway is placed between an Ipv6 over IEEE 802.15.4 network and an IP network. A Tiny Os based M2M node is allocated in its own IP address by the M2M gateway over IPv6 packets.
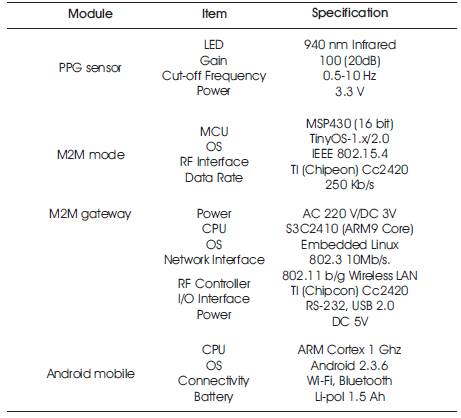
Table 1. Specification Of M2M Devices
In particular, the 6LoWPAN protocol stack is implemented on top of the IEEE 802.15.4 layer in the M2M nodes. For the transmission of packets, a higher-level protocol, namely, the LoWPAN ad hoc on-demand distance vector routing protocol is developed by the IETF group.
The measured biomedical signals are sent to the server PC through the internet by using the M2M gateway for further processing. The monitoring and analysis program, written in the C# programming language, monitors, stores, and processes the received data in the server PC. Once a data packet has been received through the M2M devices, the packet is processed, and useful data is extracted. When the data is received, an IPv6 address is identified first to ensure that the aggregated data has been sent from the correct M2M device source.
Then, the received data is scanned to ensure the data packet which is a complete packet. This program continuously monitors not only biomedical signals such as the PPG signals and oxygen saturation data acquired by wearable sensors, but also information related to M2M devices, such as communication settings and IPv6 addresses, in real-time. Further, it sends the received data to the Android mobile device to support the mobile healthcare monitoring system wirelessly after emulator testing. The mobile monitoring program was implemented and tested on the Android mobile device (Samsung Galaxy S,Korea) [21] running a 1 GHz ARM processor (Cortex A8, Hummingbird) and Android OS version 2.3.6. Through the wired or wireless internet, the server is able to connect to different types of mobile devices and various development testing can be performed on it.
Practical tests have been conducted to evaluate the real time performance of the wireless M2M healthcare system. In particular, an experiment was carried out in which one of the authors wore a wearable sensor on his wrist to perform real-time monitoring for 10 minutes. The M2M node, which is connected to the wearable sensors placed on the patient's body to collect health parameters, further transfers the data to the M2M gateway. The M2M node stores the measured signals in a buffer. Each PPG waveform consumes 25 bytes of data packets. The total 29 bytes of a 6LoWPAN packet, except the header, are included in the payload: 2 bytes for the node ID, 2 bytes for the sensor type, and 25 bytes for data. The M2M gateway is the medium between the 6LoWPAN and the internet, that delivers the packets containing the PPG signals.
The M2M gateway provides reliable IPv6 communication to transmit a patient's biomedical signals to a doctor or server via the internet. Utilizing IPv6 with the IEEE 802.15.4 standard is a special match of the two technologies. All packets transmitted through the internet are verified in the server monitoring program. All the transmitted packets are received via the User Datagram Protocol (UDP) communication in the server and the monitoring program stores its value in a database and plots all the measured biomedical signals dynamically. Various algorithms are combined and implemented as mobile application software with the Java Android language to handle all the processes from the server. The query processes handle the communication between the server and Android mobile device to display the biomedical signals graphically on a mobile screen in real time. The monitoring program also shows the record of sensing values and relevant personal information, such as a PPG waveform display and heart rate, the IPv6 address of the M2M node, the IPv6 address of the M2M gateway, the server IP, and buttons for the initiation and termination of a monitoring activity. This program is also accessible to a client PC with an IPv4 address. The server PC can share the measured signals with any internet-connected client, such as a desktop, a laptop, a tablet PC, or a mobile device, provided that the client has a fixed IPv4 address. All the transmitted data are saved for further monitoring and analysis. Firstly, to support the healthcare service, the Heart Rate Variability (HRV) analysis in the time and frequency domains extracted from the PPG signals –defined as the constant changes of the interval between the heart rates – is performed on the server for the purpose of effectively monitoring the patient's health condition [22]–[24]. The HRV is regulated predominantly by the Autonomic Nervous System (ANS) as an indicator of an individual's abilities, which describes the nerves concerned with the regulation of bodily functions without volition or consciousness. The ANS is influenced by sympathetic and parasympathetic nerves – sympathetic nerves excite the heart, increasing the Heart Rate (HR), and parasympathetic nerves reduce the heart rate [25]- [28]. By accurately measuring HRV signals on the server, the detected variation can be used to determine the psychological stress and fatigue of the body as shown in Figure 2.
Figure 2. Android emulator test for monitoring physiological stress and fatigue on the body.
Two test subjects (male, 28 and male, 32) without any heart disease were recruited for a 10-minute short-term test and a one hour long-term test. Subjects were asked to overwork and felt drowsy and entered into a mentally and physically stressed state. For the analysis of HRV signals in the time domain, the parameters of mean HR, Standard Deviation Normal to Normal (SDNN), and Root Mean Square of Successive Differences (RMSSD) were interpreted to estimate the health condition in normal and stressed states. The correlation of SDNN and RMSSD was significantly verified to explain the different patterns between the normal and stressed states. From the time domain analysis, quite uniform and stable HRV signals were extracted by the activation of parasympathetic nerves in the stressed state. In contrast, unstable HRV signals, which indicate that the patient's body is resistant to external interruption, are extracted in the normal state. The frequency domain analysis, which involves the use of the Power Spectrum Density (PSD) method to show how power distributes as a function of frequency, accordingly illustrates the likelihood of emotions associated with stress.
Three main spectral components are required for spectrum power indicator analysis: Very Low-Frequency (VLF), Low Frequency (LF), and High-Frequency (HF) components, which are usually obtained via the PSD analysis in absolute values of power. The representation of LF and HF power components emphasizes the controlled and balanced behavior of the two branches of the ANS and is quoted with the absolute values of the total LF and HF power components. Secondly, to support the mobile monitoring service, monitoring tests are required by using the Android emulator in the server before installation on the mobile device. Figure 3 shows the appearance of the Android mobile during monitoring. The Android Software Development Kit (SDK) provides emulators that can mimic a variety of Android versions, screen dimensions and phone behaviors. Although the emulator runs a bit slower than a real phone, it provides adequate support for all the features and lifecycle events, including persistent state and writing local files, and launches automatically from Eclipse. The Android emulator tests have been conducted for the monitoring application using the measured PPG signals. After testing the monitoring application with the Android emulator, the monitoring application was easily installed on the Android mobile by a direct cable or the Android Market. For the real tests, a Samsung Galaxy S model based on the Android OS was used to monitor the biomedical signals, the IPv6 address of the M2M node, the HR, and the blood oxygen saturation. The sampling rate of PPG signals in this system is 75 Hz; 15 data packets, each consisting of 5 units of the PPG data, are sent within 1 second. The waveform display in this monitoring application has a large screen, and so provides a clear visualization graphic for the user within any internet connected area. In addition, we would like to add that the popularity of mobile application stores (e.g., the Apple App Store and the Android Market) has opened an effective software delivery channel whereby a healthcare application can be installed in seconds, further lowering the barrier to user adoption. We expect that in the near future it will be possible to deliver production-quality healthcare applications globally with near zero user effort and with universal access.

Figure 3. Appearance of the Android mobile during monitoring.
A wireless M2M healthcare solution using the Android mobile devices is successfully implemented in a global network with the help of the IPv6 technique. The M2M devices are designed and used for the measurement of PPG signals and their transmission to a server PC through the IP-enabled internet, while the Android mobile device is used to provide a mobile healthcare service by means of an Android application running on a Samsung Galaxy S device with wireless internet access. By combining the 6LoWPAN and mobile communication techniques, significant network extension and higher accessibility of M2M devices had been achieved. With the use of comfortable wearable sensors in global areas, the proposed M2M healthcare system promises to improve the flexibility and scalability of healthcare applications. In addition, an Android mobile healthcare application can be deployed on mobile devices, such as smart phones, tablet PCs, and laptops to monitor biomedical signals in real time for healthcare services. Based on our results, we conclude that, with the evolution of network integration and the management of embedded devices operating multimodal tasks, a more precise and universal healthcare service scheme can be realized.